引言
遗传基因的突变、缺失或异常表达会干扰骨骼发育的信号传导通路,使骨骼形态与结构的构建出现偏差,在胎儿发育的关键孕中期,外部环境因素影响显著[1].辐射可破坏细胞DNA,导致基因突变;致畸药物会干扰细胞的正常代谢与分化;致病微生物感染可能引发炎症反应,阻碍骨骼正常发育进程;不良生活习惯如孕妇吸烟、酗酒等,会改变胎儿的宫内环境,影响骨骼生长所需的营养供应与激素平衡[2-
1 资料与方法
1.1 一般资料
选取2021年1月~2024年1月期间在我院经引产或分娩后证实为胎儿脊柱畸形的孕中期妇女58例作为研究对象,所有孕妇于孕20周时接受产前B超检查,于孕21周时接受MRI检查.孕妇年龄范围21~40岁,平均年龄(30.58±5.63)岁,孕周范围18~24周,平均孕周(21.35±3.06)周,初产妇31例,经产妇27例.纳入标准:所有孕妇均为单胎妊娠且处于孕中期,认知功能正常,配合依从性良好,符合胎儿骨骼畸形的诊断标准[7]即(1)胎儿的股骨长或肱骨长小于同期正常孕龄的4个标准差;(2)胎儿股骨长/腹围比值<0.16;(3)胎儿的四肢长度明显短于正常孕龄的胎儿,即股骨和肱骨长度低于同孕龄正常胎儿的-2个标准差;(4)胎儿长骨(如股骨、肱骨)出现异常的弯曲形态.排除标准:有严重的药物滥用史;患有心、肝、肾等严重脏器病变;合并高血压、糖尿病;甲状腺功能异常;存在吸烟、吸毒等不良生活习惯;存在异位妊娠;孕妇或其配偶存在染色体异常;中途退出实验者.所有孕妇及家属均同意胎儿影像学检查.本文所行研究符合我院伦理委员会审核标准(批准文号:2023-040-01).
1.2 方法
图像分析由两名5年以上产科及新生儿科影像学诊断经验的医师以双盲法进行胎儿B超及MRI描述和诊断,意见不一致时经科室集体会诊决定.
B超检查使用彩色多普勒超声诊断仪(上海聚慕医疗器械有限公司,型号AccuvlxA30),孕妇仰卧位,暴露腹部,凸阵探头频率设置为3~5 mHz,对胎儿羊水、脐带、胎盘位置及双径、头围、腹围、股骨长、肱骨长等进行常规检查,然后全面扫描胎儿头颈部、四肢、脊柱、胸腔、肺部及内脏,通过测量股骨长与腹围的比值和长骨的生长速度,重点关注胎儿的肱骨、股骨、骨盆和腰椎等部位的发育情况,以对胎儿的骨骼畸形状况进行评估.
MRI检查使用超导型MR扫描仪(德国西门子公司,型号Siemens Magnetom Skyra 3.0T),孕妇仰卧位,暴露腹部,于孕妇中下腹、盆腔冠状位定位像基础上,对胎儿头颅、脊柱、四肢、骨盆、四肢等部位进行轴位、冠状位和矢状位扫描.半傅里叶采集单次激发快速自旋回波序列扫描参数:矩阵256×208,视场角(field of view,FOV)44 cm×44 cm,视野380 mm×380 mm,重复时间(repetition time,TR)2 000 ms, 回波时间(echo time,TE)80 ms,层数16~20层.快速稳态进动采集成像序列扫描参数:矩阵225×225,FOV 44 cm×44 cm,视野380 mm×380mm,TR 1.0 ms, TE 2.0 ms,层数16~20层.弥散加权成像扫描参数:矩阵225×225,FOV 30 cm×30 cm,视野380 mm×380 mm,TR 2 000 ms, TE 80 ms,层数16~20层.快速扰相梯度回波序列扫描参数:矩阵320×190,FOV 22 cm×34 cm,视野380 mm×380 mm,TR 120 ms, TE 4 ms,层数16~20层,全面扫描孕妇整个子宫.
1.3 观察指标
对所有孕妇进行跟踪随访,记录和统计引产、正常生产及剖宫产情况,评估妊娠结局.以引产或分娩后的结果为金标准,对比B超检查、MRI检查方法的诊断效能.观察两种检查方法的影像质量,影像质量优表现为:具备适宜影像密度,胎儿骨骼结构和周围结构清晰可见,无阴影重叠,可完整将检查部位显示于影像照片上;影像质量良表现为:影像密度一般,胎儿骨骼结构和周围结构可显示,影像存在少量阴影分布,但不影响整体检查结果;影像质量差表现为:影像密度差,无法确定胎儿骨骼结构和周围结构情况,影像存在明显阴影分布,无法准确读片,需重新检查.总优良率=(优例数+良例数)/总例数×100%.
1.4 统计学方法
本次研究统计学纳入SPSS26.0软件处理,数据符合正态分布,计量资料、计数资料分别以均数±标准差(
2 结果
2.1 B超、MRI检查情况和妊娠结局比较
本研究中,以引产或分娩后的结果为金标准,58例胎儿均被证实存在脊柱畸形.B超检查共检出胎儿脊柱畸形46例,诊断符合率为79.31%(46/58).MRI检查共检出胎儿脊柱畸形55例,诊断符合率为94.83%(55/58).MRI检查对胎儿脊柱畸形的诊断符合率高于B超检查(χ2=6.202,P=0.013).从最终妊娠结局来看,58例孕妇中引产3例、正常生产28例、剖宫产27例.在引产建议方面,MRI建议引产3例,均与实际引产结果相符,其引产建议的诊断符合率为100.00%(3/3);而B超建议引产10例,其中3例与实际引产结果一致,引产建议的诊断符合率为30.00%(3/10).由此可见,在引产建议的准确性上,MRI优于B超,更贴合实际妊娠结局.
2.2 MRI诊断价值分析
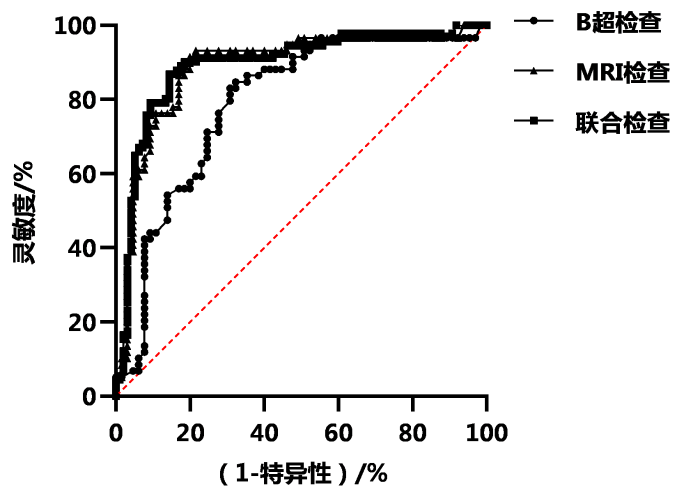
表1 ROC曲线分析B超、MRI的诊断价值
Table 1
| 检查方式 | AUC | 灵敏度 | 特异性 | 约登指数 | 标准误 | P值 | 95%CI |
|---|---|---|---|---|---|---|---|
| B超检查 | 0.792 | 81.65% | 77.83% | 0.595 | 0.12 | <0.001 | 0.705~0.808 |
| MRI检查 | 0.902 | 90.17% | 88.53% | 0.787 | 0.15 | <0.001 | 0.839~0.943 |
| 联合检查 | 0.925 | 90.39% | 89.04% | 0.794 | 0.10 | <0.001 | 0.894~0.944 |
注:灵敏度指检测方法正确识别真实患病病例的能力;特异性指检测方法正确排除非病例的能力;约登指数是综合评价诊断效能的指标,范围为0~1,越接近1诊断价值越高;95%CI表示95%置信区间,反映指标估计值的可信范围,区间越窄精度越高. 具体计算公式见文献[
图1
图1
ROC曲线分析B超、MRI的诊断价值
Figure 1
ROC curve analysis of diagnostic value of B-scan and MRI
2.3 不同检查方法诊断影像质量比较
B超、MRI检查影像质量总优良率分别为86.21%、96.55%,MRI检查方法的影像质量总优良率高于B超(P<0.05).不同检查方式诊断影像质量见表2.
表2 不同检查方式诊断影像质量比较(n=58)
Table 2
| 检查方式 | 优 | 良 | 差 | 优良 |
|---|---|---|---|---|
| B超检查 | 48(82.76) | 2(3.45) | 8(13.79) | 50(86.21) |
| MRI检查 | 52(89.66) | 4(6.89) | 2(3.45) | 56(96.55) |
| χ2 | 3.940 | |||
| P | 0.047 |
注:前两行数据为数量(百分占比/%)
2.4 B超、MRI检查的骨骼畸形种类比较
进一步对不同类型胎儿骨骼畸形进行检查结果显示,产前B超诊断符合率为79.31%,产前MRI诊断符合率为94.84%,MRI诊断符合率高于B超.B超、MRI检出的骨骼畸形种类见表3.
表3 B超、MRI检出的骨骼畸形种类比较
Table 3
| 骨骼畸形种类 | 实际发生例数 | B超检出例数 | MRI检出例数 |
|---|---|---|---|
| 足内翻 | 13(22.41) | 10(17.24) | 13(22.41) |
| 多(并)指、趾 | 9(15.52) | 7(12.07) | 9(15.52) |
| 手缺失 | 9(15.52) | 8(13.79) | 9(15.52) |
| 桡骨缺失 | 6(10.34) | 5(8.62) | 6(10.34) |
| 颅骨缺失 | 5(8.62) | 5(8.62) | 5(8.62) |
| 股骨不等长 | 3(5.19) | 2(3.45) | 2(3.45) |
| 尾端退化综合征 | 2(3.45) | 1(1.73) | 1(1.72) |
| 脊柱裂 | 7(12.06) | 5(8.62) | 6(10.34) |
| 骨不全 | 4(6.89) | 3(5.17) | 4(6.89) |
| 总计 | 58(100.00) | 46(79.31) | 55(94.84) |
注:括号内数据为百分占比/%
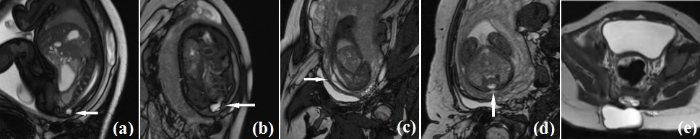
2.5 案例分析
(1)脊髓脊膜膨出畸形,孕34周B超提示胎儿骶椎椎弓距增宽并见低回声.MRI矢状及冠状位见骶尾部背侧的囊性包块,与椎管相同,呈T2高的等脑脊液信号,内部未见等低信号的脊髓组织.产后MRI证实见图2.
图2
图2
胎儿MRI扫描脊髓脊膜膨出畸形及出生后图像. (a)胎儿矢状位;(b)胎儿冠状位骶骨T2高信号囊性灶;(c)胎儿矢状位;(d)胎儿轴位见囊性成分与椎管内脑脊液相通;(e)胎儿出生后图像
Figure 2
Fetal MRI scans of myelomeningocele malformation and postnatal images. (a) Fetal sagittal position; (b) Fetal coronal position showing sacral T2 hyperintense cystic lesion; (c) Fetal sagittal position; (d) Fetal axial position showing communication between cystic component and intraspinal cerebrospinal fluid; (e) Postnatal image
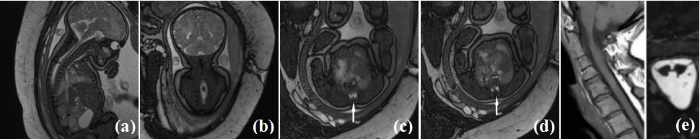
(2)脊髓纵裂畸形,孕36周,B超提示胎儿胸椎椎管内稍强回声团.MRI矢状位及冠状位见胎儿上段胸椎椎管局部扩张,脊髓膨大,椎管内异常信号.MRI横轴位见脊髓贴近椎管前壁,并分成左右两部分,脊髓后方见条状T2等低信号的嵴样分隔突向前方.产后MRI扫描证实见图3.
图3
图3
胎儿MRI扫描脊髓纵裂畸形及出生后图像. (a)胎儿矢状位;(b)胎儿冠状位图像见椎管局部扩张、脊髓膨大,内见T2低信号灶;(c)胎儿轴位;(d)胎儿轴位见脊髓被分成左右两部分;(e)胎儿出生后图像
Figure 3
Fetal MRI Scans of Diastematomyelia and Postnatal Images. (a) Fetal sagittal view; (b) Fetal coronal view showing local dilatation of the spinal canal, spinal cord enlargement, and a T2-weighted hypointense lesion inside; (c) Fetal axial view; (d) Fetal axial view showing the spinal cord divided into left and right parts; (e) Postnatal image
(3)半椎体畸形,孕26周,B超提示腰椎排列紊乱,MRI扫描SWI序列能更清晰的显示第三腰椎半椎体畸形.孕27周,当地超声提示腰椎半椎体畸形,MRI检查支持诊断,SWI及Trufi序列均显示良好,并出生后CT VRT重建后较直观显示,见图4.
图4
图4
胎儿MRI扫描半椎体畸形及出生后图像. (a)胎儿磁敏感加权成像(Susceptibility-Weighted Imaging, SWI)冠状位图像;(b)胎儿冠状位;(c)胎儿冠状位;(d)胎儿冠状位图像见第三腰椎半椎体畸形;(e)胎儿出生后CTVR(Computed Tomography Virtual Reality)重建图像
Figure 4
Fetal MRI Scans of Hemivertebra Malformation and Postnatal Images. (a) Fetal SWI coronal view; (b) Fetal coronal view; (c) Fetal coronal view; (d) Fetal coronal view showing hemivertebra malformation at the third lumbar vertebra (L3); (e) Postnatal CTVR reconstructed image
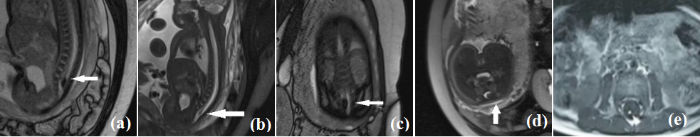
(4)脊髓栓系畸形,孕35周B超提示胎儿脊柱腰骶段椎管内可见梭型强回声团,MRI检查矢状位见脊髓圆锥位于第五腰椎以下水平,且末端增粗.冠状位显示脊髓末端呈梭形膨大,横轴位见膨大的圆锥紧贴、粘连于椎管背侧,产后MRI见增粗的并粘连的脊髓圆锥内部有T1高的脂肪信号,见图5.
图5
图5
胎儿MRI扫描脊髓栓系畸形及出生后图像. (a)胎儿矢状位;(b)胎儿矢状位;(c)胎儿冠状位,可见椎管局部扩张、脊髓末端膨大且位置低;(d)胎儿轴位,可见椎管内异常信号紧贴椎管后壁;(e)胎儿出生后MRI图像
Figure 5
Fetal MRI Scans of Tethered Cord Malformation and Postnatal Images. (a) Fetal sagittal view; (b) Fetal sagittal view; (c) Fetal coronal view showing local dilatation of the spinal canal, enlargement of the terminal spinal cord, and a low position of the terminal spinal cord; (d) Fetal axial view showing abnormal signal in the spinal canal closely adjacent to the posterior wall of the spinal canal; (e) Postnatal fetal MRI image
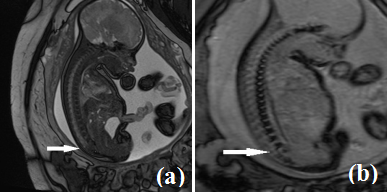
(5)尾端退化综合征畸形,孕28周B超提示骶尾椎显示不清,MRI检查发现胎儿骶尾段椎体、马尾缺如,脊背部软组织平坦,考虑胎儿尾端退化综合征,见图6.产妇经过多学科会诊后决定引产.
图6
图6
胎儿MRI扫描脊髓栓系畸形尾端退化综合征畸形. (a)胎儿矢状位;(b)胎儿矢状位可见骶尾段椎体及马尾缺如
Figure 6
Fetal MRI Scans of Tethered Cord Malformation and Caudal Regression Syndrome Malformation. (a) Fetal sagittal view; (b) Fetal sagittal view showing absence of sacrococcygeal vertebrae and cauda equina
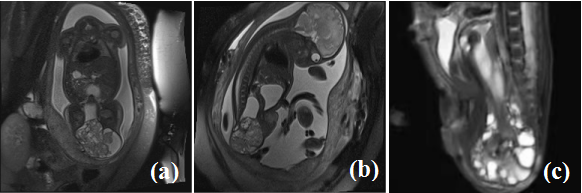
(6)骶尾部畸胎瘤畸形,胎儿26周B超提示胎儿骶尾部外凸一肿块,内含强回声,MRI胎儿尾部混杂信号肿块,与椎管未见确切关系,病灶部分位于尾椎前方、部分外凸及产后MRI见图7.
图7
图7
胎儿MRI扫描骶尾部畸胎瘤畸形及出生后图像. (a)胎儿冠状位可见骶尾部外凸的较大肿物;(b)胎儿矢状位可见骶尾部外凸的较大肿物;(c)胎儿出生后MRI图像
Figure 7
Fetal MRI Scans of Sacrococcygeal Teratoma Malformation and Postnatal Images. (a) Fetal coronal view showing a large externally protruding mass in the sacrococcygeal region; (b) Fetal sagittal view showing a large externally protruding mass in the sacrococcygeal region; (c) Postnatal fetal MRI image
3 讨论
胎儿骨骼畸形作为一种以形态结构异常为特征的先天性畸形,对人口素质影响重大,尽早诊断意义非凡[9].胎儿骨骼发育起始于胚胎期的中胚层,其发育过程主要涉及膜内成骨和软骨内成骨两种方式,膜内成骨主要发生于颅骨、面骨等扁骨,而大多数四肢长骨、脊柱等骨骼通过软骨内成骨方式发育,于胚胎早期,间充质细胞先分化形成软骨雏形,软骨细胞不断增殖、肥大,随后血管侵入,软骨基质被逐步降解,成骨细胞在残留的软骨基质上分泌骨基质并矿化,最终形成成熟的骨组织,这一复杂过程中,当对软骨细胞的增殖和分化起重要负调控作用的成纤维细胞生长因子受体3基因发生突变时,会过度激活其信号通路,抑制软骨细胞增殖,致使长骨生长受阻,引发软骨发育不全,出现骨骼畸形,影响妊娠结局,因此准确、有效的产前诊断具有十分重要的临床意义.其中B超和MRI是常用的影像学检查手段,B超操作简便、费用较低,能实时动态成像,可动态监测胎儿骨骼运动,对于辨别生理性和病理性骨骼改变意义重大[10].然而,B超存在软组织及空间分辨率低的问题,且成像质量受操作手法、羊水量、胎位等因素影响,易出现漏诊.MRI虽然检查时间长、费用高且缺乏实时动态观察能力,但它具备高软组织分辨率,能进行轴位、冠状位和矢状位等多平面成像,全方位展示胎儿骨骼细微结构与空间位置关系,有助于发现早期或隐匿性骨骼病变,成像不受胎儿体位和羊水量影响,诊断准确性和可靠性高,比如在检测胎儿脊柱裂时,MRI既能清晰显示脊柱骨性结构缺损,又能准确观察脊膜膨出、脊髓栓系等软组织病变,全面评估病变范围和严重程度[11-12].MRI凭借高软组织分辨率和多平面成像功能,清晰显示骨骼周围组织及未完全骨化结构,弥补B超不足,二者联合使用时,B超的实时动态监测与MRI的高分辨率、多平面成像优势互补,能更全面、准确地评估胎儿复杂骨骼畸形及其对周围组织的影响,为临床提供更丰富、可靠的诊断信息.
本研究以引产或分娩结果为金标准,发现B超、MRI检出的胎儿骨骼畸形例数分别为46例、55例,MRI检查方法的检出例数高于B超,凸显其在孕中期胎儿骨骼系统发育畸形诊断中的高准确性,表明孕中期进行MRI诊断是产前评估胎儿骨骼畸形的有效策略.分析原因:MRI基于原子核磁共振现象,能提供多参数、多序列成像.在观察胎儿骨骼时,其对软组织分辨力极高,不仅能清晰显示骨骼形态,还能更好地呈现骨骼周围肌肉、韧带、神经等软组织的情况,可发现一些细微的骨骼结构异常及软组织病变累及骨骼的情况,而B超主要依赖超声反射成像,在软组织分辨及复杂结构的观察上存在一定局限性,例如细微骨骼畸形易被遗漏,对复杂骨骼结构的显示也相对模糊,使得其在诊断胎儿骨骼系统发育畸形时,整体效能弱于MRI.
本研究中,B超、MRI检查方法的引产建议诊断符合率分别为30.00%、100.00%,MRI检查方法的引产诊断符合率高于B超,原因在于MRI诊断准确性更高,能发现更多B超漏诊的胎儿骨骼畸形情况.而正常生产率和剖宫产率在B超与MRI组间比较差异无统计学意义,这主要是因为分娩方式主要取决于孕妇整体身体状况、胎位、产道条件等因素,胎儿骨骼畸形诊断方法对这些分娩相关因素影响较小[15-16]. Liang[17]等研究发现,产前MRI诊断与随访出生或引产结果完全一致,认为当产前超声筛查观察到胎儿脊柱脊髓显示不清或诊断不明确时,可以选择MRI补充检查.胎儿骨骼畸形常作为全身性骨骼异常或多发畸形的局部表现,对妊娠结局影响显著,比如,多指畸形可能是13-三体综合征的局部表现,13-三体综合征胎儿常伴有严重智力障碍、心脏及其他器官发育异常等,预后极差,往往建议引产.而胎儿姿势固定可能与18-三体综合征相关,18-三体综合征胎儿多存在生长发育迟缓、多发畸形等问题,出生后生存质量极低,也多考虑终止妊娠.因此,准确诊断胎儿骨骼畸形对于判断是否存在潜在染色体异常及评估妊娠结局意义重大.有研究证实,MRI可作为胎儿畸形产前超声诊断的重要补充,有助于改善妊娠结局[18].Zhang[19]等研究显示,90例孕妇经分娩或引产证实,MRI诊断畸形胎儿73个,高于四维超声诊断的67个,可为预测孕妇的妊娠结局提供有力帮助.此外,本研究通过ROC曲线分析,MRI的AUC为0.902,也表明其较高的诊断价值.相关文献报道[20],MRI诊断的敏感度为91.23%,特异性为83.33%,诊断符合率为88.51%,与分娩病理金标准具有一致性,剖宫产率、不良妊娠结局发生率均高于健康对照组,认为产前MRI诊断妊娠期胎盘植入具有较高的诊断准确性,可为临床不良妊娠结局诊断提供数据性指导.Zhen[21]等认为,产前超声联合MRI诊断胎儿闭合性脊柱裂的AUC为0.912,MRI可作为产前超声的补充检查方式,二者联合应用可提高对胎儿闭合性脊柱裂的诊断效能.
基于前文对B超和MRI在胎儿骨骼畸形诊断符合率等情况的分析,在临床干预及诊断优化上,需充分考量MRI的诊断结果.对于MRI诊断出的轻度多指(趾)畸形这类对胎儿生长发育影响轻微的骨骼异常,因其不影响胎儿基本生存质量,可建议继续妊娠.同时,为孕妇提供全面的病情说明,涵盖畸形成因、发展态势及产后治疗方案,联合多学科专家制定出生后手术矫正等早期干预规划,切实保障优生优育.若MRI确诊为先天性脊柱侧弯等严重但可通过医疗手段有效治疗的畸形,医生需与家属深度沟通产后治疗细节,给予心理安抚,协助获取治疗资源.在妊娠后期密切监测胎儿状况,确保出生后能及时介入治疗,改善预后.面对严重成骨不全症等致死性或难以治愈的骨骼畸形,医生应如实告知病情及预后,尊重家属自主选择.若选择引产,医院应给予人文关怀,避免缺陷儿出生.先以超声的实时动态与操作简便优势进行初步筛查,发现可疑再用MRI高分辨率和多平面成像详细评估,优势互补.实现对胎儿骨骼畸形的精准诊断.本研究存在一定不足,例如选择样本的数量相对较少,研究调查时间较短,可能对结果产生一定影响,故后续将通过扩大样本量、延长研究时间,对其应用需要更进一步的研究论证,为后续研究提供直接的指导价值.
4 结论
MRI在孕中期胎儿骨骼畸形诊断中的价值较高,可为孕妇及家属提供胎儿骨骼可靠信息,有利于改善孕中期孕妇妊娠结局,为优生优育提供保障,值得临床推广应用.
利益冲突
无
参考文献
Genetic analysis of 55 cases with fetal skeletal dysplasia
[J].
DOI:10.1186/s13023-022-02559-4
PMID:36352425
[本文引用: 1]

Fetal skeletal dysplasia (SD) is a common congenital disability comprising a complex group of skeletal disorders with substantial clinical and genetic heterogeneity. Many of these defects are detected prenatally using ultrasound (US). However, the diagnostic accuracy of the US is limited.We recruited 55 unrelated fetuses with US-detected skeletal anomalies and performed sequential tests using copy number variation sequencing, targeted skeletal gene panel sequencing, or whole exome sequencing. The detected variants were validated using Sanger sequencing or multiplex ligation-dependent probe amplification. We conducted breakpoint analysis and structural modeling of variants possibly involved in fetal SD.A definitive diagnosis was achieved in 81.82% of affected fetuses (45/55). We identified chromosomal abnormalities in seven cases and 36 variants, of which 18 were novel pathogenic or likely pathogenic in 11 genes in 38 cases. De novo variants were identified in 27 cases (71.05%, 27/38), and one gonosomal mosaicism variant was found in the mother of one fetus. Our case examples demonstrated the high heterogeneity of fetal SDs and the rare fetal SD-associated challenges.Careful clinical evaluation of fetuses with SD can guide appropriate molecular testing. Our study extends the SD-associated pathogenic variant spectrum and provides useful genetic counselling guidance and an accurate prenatal diagnosis strategy.© 2022. The Author(s).
Three-dimensional bone imaging diagnosis of fetal rib fusion costospinal junction deformity: a case report
[J].
三维骨骼成像诊断胎儿肋骨融合肋脊连接畸形分析1例
[J].
Prenatal three-dimensional ultrasonography and chromosomal microarray analysis for screening fetal skeletal abnormalities and genetic etiology analysis
[J].
产前三维超声与染色体微阵列分析技术筛查骨骼畸形异常胎儿及遗传学病因分析
[J].
Application of magnetic resonance imaging in fetal central nervous system
[J].
磁共振成像在胎儿中枢神经系统中的应用进展
[J].
The value of magnetic sensitivity weighted imaging for fetal spinal anatomic and developmental malformation
[J].
磁敏感加权成像显示胎儿脊柱解剖及发育畸形的价值
[J].
Correlation analysis of prenatal ultrasound screening for fetal bone malformation and chromosomal microarray analysis
[J].
产前超声筛查胎儿骨骼畸形与染色体微阵列分析特征的相关性分析
[J].
ROC-ing along: Evaluation and interpretation of receiver operating characteristic curves
[J].
Prenatal diagnosis of fetal skeletal dysplasia using targeted next-generation sequencing: an analysis of 30 cases
[J].
DOI:10.1186/s13000-019-0853-x
PMID:31299979
[本文引用: 1]

This study aims to provide genetic diagnoses for 30 cases of fetal skeletal dysplasia, and a molecular basis for the future prenatal diagnosis of fetal skeletal dysplasia.A total of 30 cases of fetal skeletal dysplasia detected with ultrasound between January 2014 and June 2017 were analyzed. Among these fetuses, 15 fetuses had local skeletal malformations, while 15 fetuses had short limb malformations. Samples of fetal umbilical cord blood, amniotic fluid, and/or aborted tissue were collected from all cases. Karyotyping, whole genome sequencing, and targeted next-generation sequencing of skeletal disease-related pathogenic genes were performed, as needed. Blood samples were taken from the parents for verification using Sanger sequencing.Among the 30 cases of fetal skeletal dysplasia, two cases were diagnosed with trisomy 18. However, none of these cases were identified with any microdeletions or microreplications associated with skeletal dysplasia. Among the 28 chromosomally normal cases with fetal skeletal dysplasia, 21 cases were detected with mutations in genes related to skeletal diseases. Furthermore, collagen gene mutations were detected in six fetuses with short limb malformations, while heterozygous disease-causing mutations in the fibroblast growth factor receptor 3 (FGFR3) gene were detected in seven fetuses. The remaining fetuses carried mutations in other various genes, including tumor protein p63 (TP63), cholestenol delta-isomerase (EBP), cholinergic receptor nicotinic gamma subunit (CHRNG), filamin B (FLNB), and SRY-box 9 (SOX9). Three compound heterozygous mutations in CHRNG, COL11A2 and SOX9 were carried by phenotypically healthy parents.Targeted next-generation sequencing can significantly improve the prenatal diagnoses of fetal skeletal dysplasia, providing parents with more precision medicine, and improved genetic counseling.
Ultrasound diagnosis and genetic analysis of congenital skeletal malformations in fetuses
[J].
先天性骨骼畸形胎儿的超声诊断和遗传学分析
[J].
Fetal body MRI for fetal and perinatal management
[J].
Fetal structural anomalies diagnosed during the first, second and third trimesters of pregnancy using ultrasonography: a retrospective cohort study
[J].
DOI:S1516-31802019000500391
PMID:31939566
[本文引用: 1]

The prevalence of congenital abnormalities in general populations is approximately 3-5%. One of the most important applications of obstetric ultrasound is in detection of fetal structural defects.To assess fetal structural anomalies diagnosed using ultrasound in the three trimesters of pregnancy.Retrospective cohort study at the Mário Palmério University Hospital of the University of Uberaba (Universidade de Uberaba, UNIUBE), from March 2014 to December 2016.Ultrasound data at gestational weeks 11-13 + 6, 20-24 and 32-36 were recorded to identify fetal anomalies in each trimester and in the postnatal period. The primary outcome measurements were sensitivity, specificity, positive predictive value and negative predictive value for detection of fetal anomalies and their prevalence.The prevalence of anomalies detected using ultrasound was 2.95% in the prenatal period and 7.24% in the postnatal period. The fetal anomalies most frequently diagnosed using ultrasound in the three trimesters were genitourinary tract anomalies, with a prevalence of 27.8%. Cardiac anomalies were diagnosed more often in the postnatal period, accounting for 51.0% of all cases. High specificity, negative predictive value and accuracy of ultrasound were observed in all three trimesters of pregnancy.Ultrasound is safe and has utility for detecting fetal anomalies that are associated with high rates of morbidity and mortality. However, the low sensitivity of ultrasound for detecting fetal anomalies in unselected populations limits its utility for providing reassurance to examiners and to pregnant women with normal results.
Value of ultrasonography in the diagnosis of skeletal deformity of limbs of fetus in the second trimester
[J].
中孕期胎儿肢体骨骼畸形的超声诊断价值
[J].
Application of prenatal ultrasound and MRI in the diagnosis of fetal malformation
[J].
产前超声和MRI在诊断胎儿畸形中的应用
[J].
The clinical value of MRI in the diagnosis of fetal malformation
[J].
MRI对胎儿畸形诊断的临床价值
[J].
Comparative study on imaging quality of different magnetic resonance imaging sequences in prenatal fetal diagnosis
[J].
磁共振不同成像序列在产前胎儿诊断成像质量的比较研究
[J].
MRI diagnosis of fetal spinal cord malformation and sequence selection
[J].
MRI诊断胎儿脊柱脊髓畸形及序列选择
[J].
Analysis of clinical application value of transabdominal ultrasonography and MRI in prenatal fetal malformation
[J].
经腹壁超声、MRI检查在产前胎儿畸形中的临床应用价值分析
[J].
Clinical diagnostic value of fourdimensional ultrasound combined with MRI in fetal malformation in second trimester and pregnancy outcomes
[J].
四维超声联合MRI成像对中孕期胎儿畸形的临床诊断价值及其妊娠结局
[J].
Correlation between MRI diagnostic value of placenta implantation during pregnancy and pregnancy outcome
[J].
妊娠期胎盘植入的MRI诊断价值与妊娠结局的相关性
[J].